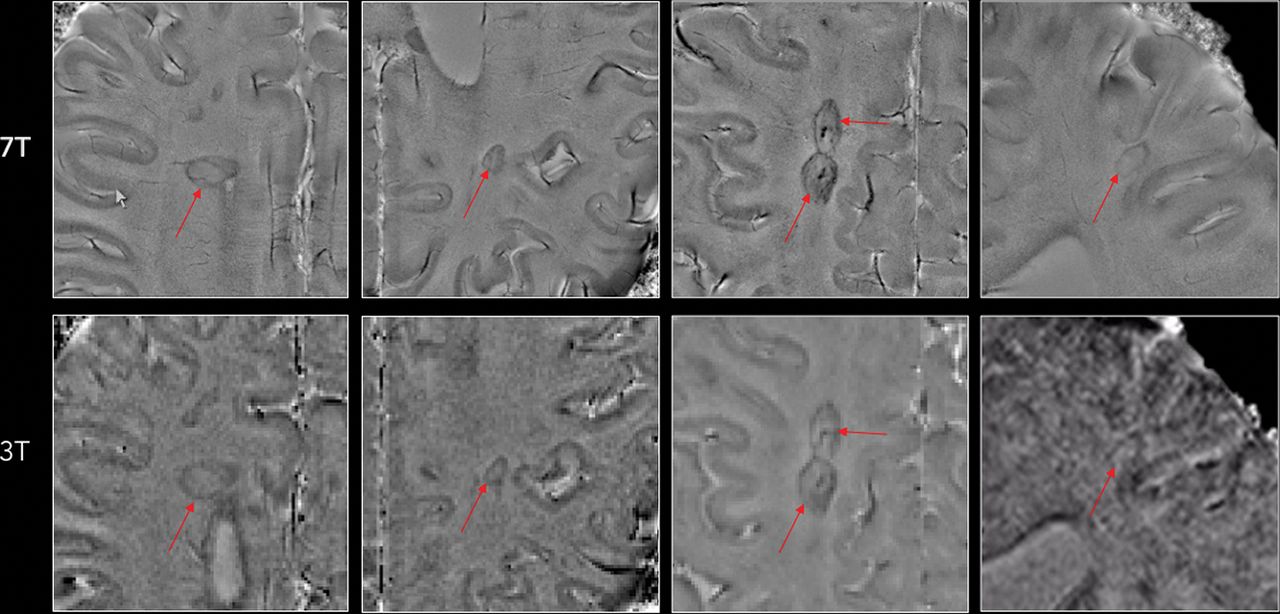
A chronic Active Lesion has a demyelinated centre and rim of myelin damage/removal by macrophages. These can be seen on a 7T magnetic resonance imaging scanner, but this study shows they can also be seen on a lower power 3T machine. If you can see it then you can monitor it.
BACKGROUND AND PURPOSE: MR imaging-pathologic studies have reported that paramagnetic rims on 7T susceptibility-based MR imaging identify, in vivo, the subset of MS lesions with compartmentalized inflammation at the lesion edge and associated remyelination failure. Here, we assessed the reliability of detecting these rims on high-resolution 3T phase images.
MATERIALS AND METHODS: High-resolution T2* and phase MR imaging was collected in 20 patients with MS at 3T (3D segmented EPI, 0.65 mm3) and 7T (2D gradient-echo, 0.2 × 0.2 × 1 mm) MR imaging. In each case, 5 discrete chronic (non-enhancing) MS lesions were selected on T2 FLAIR images for rim evaluation. Five raters experienced in MS imaging contributed to the rim assessment, of whom 3 worked independently on 3T data, and 2, on 7T data. Consensus agreement was reached for both 3T and 7T rim evaluations. Discrepancies between 3T and 7T were discussed, and consensus was reached.
RESULTS: Phase rims were seen in 34 lesions at 7T and in 36 lesions at 3T by consensus. Inter- and intrarater reliability were "substantial/good" both at 3T and 7T analysis (Cohen κ, >0.71). Based on consensus agreement, the reliability of rim visualization at 3T versus 7T was 0.78 (κ) with a pair-wise agreement of 90%. More lesions were judged to be false-positive or false-negative at 3T than at 7T.
CONCLUSIONS: Nearly all 7T paramagnetic rims can also be seen at 3T. Imaging at 3T opens the possibility of implementing paramagnetic rims as an outcome measure in multicenter, MR imaging-based clinical trials aimed at treating perilesional persistent inflammation and its potential effects on remyelination.
http://www.ajnr.org/content/ajnr/early/2018/05/03/ajnr.A5660/F2.large.jpg?width=800&height=600&carousel=1